
Senti Biosciences’ CEO Tim Lu talks about the challenges facing cell therapies -- and how we can overcome them
Senti Biosciences’ CEO Tim Lu talks about the challenges facing cell therapies -- and how we can overcome them
It is ironic that to eliminate the poisonous cancer cells from the human body, we turn, in most cases, to another set of poisons: radiation and chemotherapy. For years, patients and doctors alike have begged for and predicted our exit from the so-called stone age of cancer treatment. With the advent of alternative therapies like chimeric antigen receptor T-cell (CAR-T) therapies, we are moving closer to such a future.CAR-T has been revolutionary because it in essence “primes” the patient’s immune system -- T cells, specifically -- to better recognize and target cancerous cells. Cells are removed from the patient’s body and, in the lab, they are genetically modified -- usually through a viral vector -- to express a receptor for an antigen expressed by cancer cells before being transfused back into the patient’s bloodstream. One of the biggest issues with this approach, however, is that the targeted antigen is also expressed by non-cancerous cells. Like chemotherapy and radiation, current CAR-T therapies often kill healthy cells along with cancerous ones.Yet this is no reason to give up on using living cells to target cancer.Tim Lu, co-founder and CEO of Senti Biosciences -- a Bay Area-based company focused on the next generation of gene and cell therapies -- thinks that living cells are a critical component of the future of cancer treatment. And he believes that synthetic biology is an ideal way to address the challenges facing cell therapies and bring them to the clinic.
The biological challenges of cell therapies
Lu sees two challenges facing cell therapies today: biological challenges (i.e., getting them to work specifically and safely) and translational challenges (i.e., getting them into the clinic quickly). Not only could cell therapies stand to benefit from targeting different -- or even better, multiple -- antigens to discriminate cancerous cells from normal ones, but they currently suffer from the inability to target solid tumors, rendering them ineffective for a large proportion of cancers. The biological premise is simple: solid tumors can turn the anti-cancer immune response down or even completely off -- a critical blow to an immune cell-based therapy.If cell therapies are to make it to the clinic, they also need to be relatively safe. Because these therapies are very potent, programming them to respond only when needed, to be able to attenuate and control their activities, or to be able to turn them off when they’re no longer needed are critical safety measures that should be built in to any cell-based therapy.These are not easy challenges to overcome, to be sure, but Senti is tackling them head-on using a powerful synthetic biology tool: gene circuits.
Gene circuits: the key to fine-tuned cell therapies
Gene circuits are precise, multi-component biological constructs that program living cells to perform logical functions -- just like electronic circuits. Simply put, the engineered gene circuits sense and react to inputs, such as regulatory signals, and then produce a specified output, such as changes in protein levels. This enables living cells to be active only in specific locations of the body or when experiencing certain disease states, rather than systemically or constitutively staying active.

Image source: Senti BiosciencesSo how does this translate to cell therapies for cancer? Take, for example, the problem of discriminating between normal and cancerous cells.“With synthetic gene circuits, you can actually start doing things like recognize two different antigens and only trigger when one is there -- target antigen A-expressing cells but not normal cells that express antigen A and B, for example” says Lu. “That type of logic opens up a wide range of target combinations, because you can start putting two targets, three targets together in a way that allows you to be more specific at discriminating cancer cells from normal ones -- enabling enhanced therapeutic activity while minimizing toxicity.”Gene circuits in living cells add a unique advantage compared to traditional antibody-based therapies, Lu adds. “With proteins, you're quite limited in the types of multi-antigen targeting that you can do, whereas with cells you have a great amount of flexibility -- and it doesn't have to be antigens. You could make cells that recognize a single antigen and also respond to a microenvironment signal the tumor,” he says. This could facilitate cell-based therapies for solid tumors, where the microenvironment is full of immunosuppressive signals.Another approach to targeting solid tumors is to program cells to produce different immunomodulators, reducing the tumor’s ability to suppress the immune system and ensure a robust anti-cancer immune response. Senti is focusing on how to do this in a localized, controlled way, by building gene circuits that not only produce the desired combination of immunomodulators but that also recognize microenvironment components that trigger their response when -- and where -- needed.

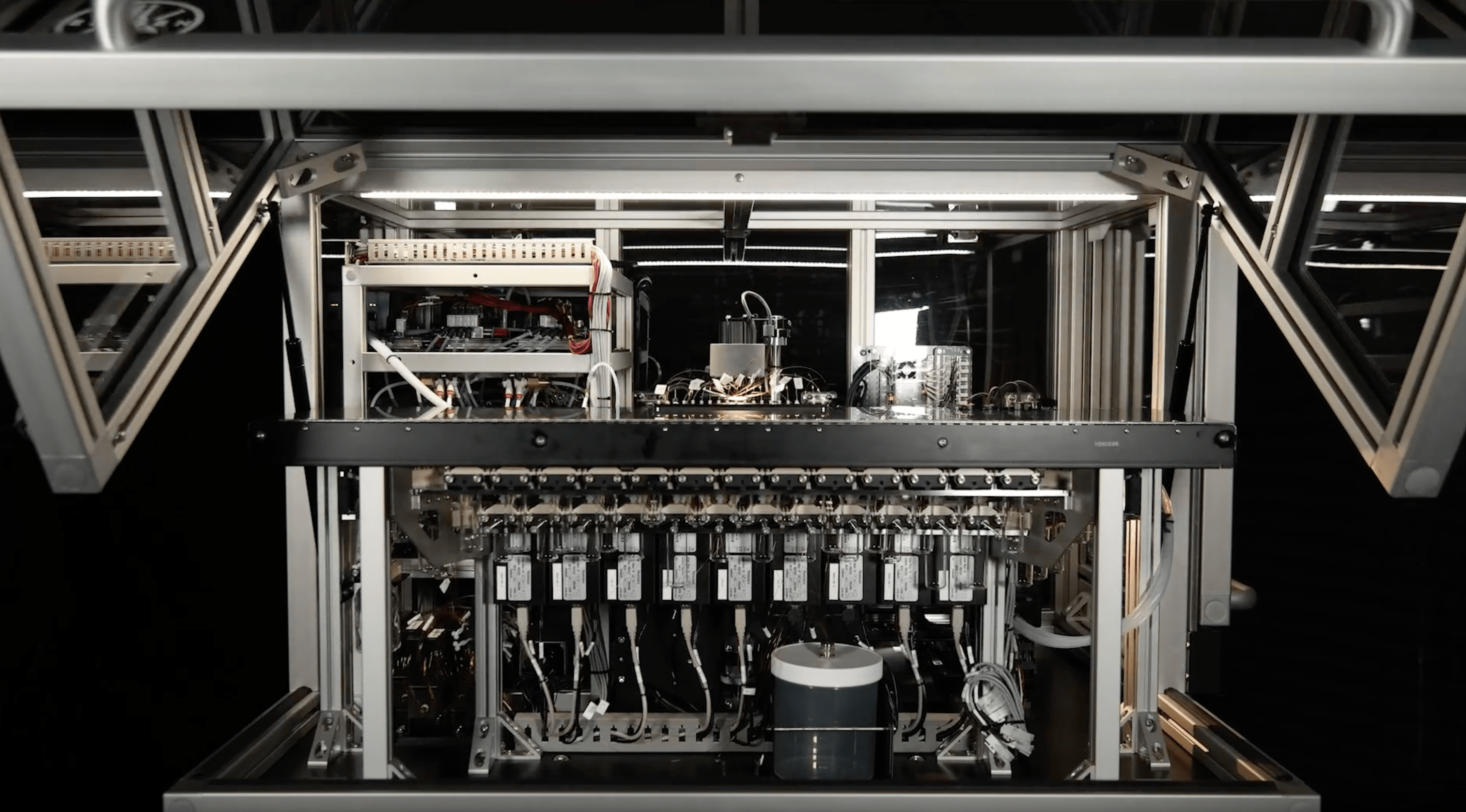
Gene circuits can program cells to go directly to a tumor and trigger an immune response, leading to localized anti-tumor immune responses. Image source: Senti BiosciencesGene circuits are also faster to design and tweak than other methods. “Think about the speed at which you can design gene circuits,” posits Lu. “It's becoming faster and faster with better DNA synthesis technologies, and so your ability to iterate and create a new design is accelerating, especially compared to traditional drug molecules. We’ve even thought about situations where you do an exploratory clinical trial with your cells and learn from the data to quickly go back and redesign the system and try to make it better. Synthetic biology has that opportunity to give you rapid iteration and diversification,” he says.But there are still significant bottlenecks to bring cell therapies to the clinic, even with approaches like gene circuits that can target some of the biological challenges to making them function appropriately.
The practical translational challenges of cell therapies
Currently approved engineered cell therapies are not cheap to manufacture. One of the biggest costs associated with cell therapies comes from making the viral vectors needed to deliver the modified gene set. Some feel that non-cell-based approaches are a better approach, and companies are actively working on bi-specific antibody approaches as an alternative to cell-based approaches. But Lu isn’t convinced that going completely cell-free is the best solution.“Cells give you a couple of different, really unique features -- cells are naturally suited to do signal integration and logic computing. I think it'd be very challenging to do that solely from a protein engineering perspective,” he says. Instead, moving away from using viral vectors, using off-the-shelf cell sources, and looking beyond T cells into other cell types, such as mesenchymal stromal cells, natural killer cells, and macrophages, could represent big time and money savings.And, the right disease model is critical for success -- and for reducing the cost associated with developing a therapy. Lu says that genetic modification of animal models, such as mouse or large animal models of disease, is the perfect application for gene circuit technology.“If we actually had good models of disease, the failure rate would be lower. The analogy I like to use is ... before you design a complex CPU, you don't just go ahead and build it, you simulate it, a lot. It's through that simulation process that you can be really confident that whatever you've designed will actually translate once you manufacture it. We don't really have accurate simulators in biology at this point,” he says -- and they are ripe for development.For example, modeling biological systems can be improved through cell lineage tracking -- determining where each cell in a tumor originated from and how it got there. Lu’s group at MIT and others have been developing genetic recorders using CRISPR, enabling them to record cell lineages and track molecular events at the single cell level.“Imagine coupling those two pieces of information together -- tracking where cells are coming from, but also what is the microenvironment they encounter along the way. You can get a lot of information about how tumors develop over time,” says Lu.Furthermore, gene circuits can be used to create models where biological changes are triggered at the right time and place to represent human disease. More accurate models will enable therapies to be iteratively optimized in the lab before testing them in people.
Closer to the clinic than ever
But none of this matters if you can’t get clinicians on board. The gatekeeper to patient health, the clinician needs to be convinced of the utility of cell-based therapies. One of the biggest issues facing pharmaceutical drugs today is their failure to translate once applied to human models. To mitigate this issue, the Senti team is addressing targets and mechanisms that have been tested in patients before but failed due to toxicity or the inability to deliver drugs to the right place -- and they have several candidate therapies that they aim to introduce to the clinic.In general, clinicians are excited about the potential of cell-based therapies, says Lu. Their major concerns are the complexity of the treatment regimen and ability to provide access to broader patient populations. For example, some current cell therapies require a stay in the ICU due to the potentially serious side effects associated with the treatment -- so these therapies don’t just suffer from the cost of manufacture, but also the resource costs to the hospitals in which they’re used. The hope is that in the future, cell therapy will be as quick as dialysis -- an outpatient procedure with minimal side effects.As for Tim Lu and the rest of the Senti team, while their focus is on targeting cancer and getting their first therapies into the clinic in the next couple of years, they haven’t lost sight of the bigger picture.“Today people talk about cures for multiple myeloma and acute lymphoblastic leukemia. That was not imaginable before,” he says. It’s a future that is now possible, one that he works for each and every day. And with the help of synthetic biology and the power of living cells, we may soon exit the stone age of cancer treatment once and for all.Tim Lu will be speaking on engineered cell therapies at SynBioBeta 2019 October 1-3 in San Francisco, CA.



.svg)





.png)

.jpg)
.gif)