Engineered Human Therapies
Taming the T Cells: A Revolutionary Step in Car T-Cell Therapy
Yale researchers have discovered a way to curb the self-destructive tendencies of engineered T cells in CAR T-cell therapy, potentially revolutionizing treatments for lymphoma and leukemia
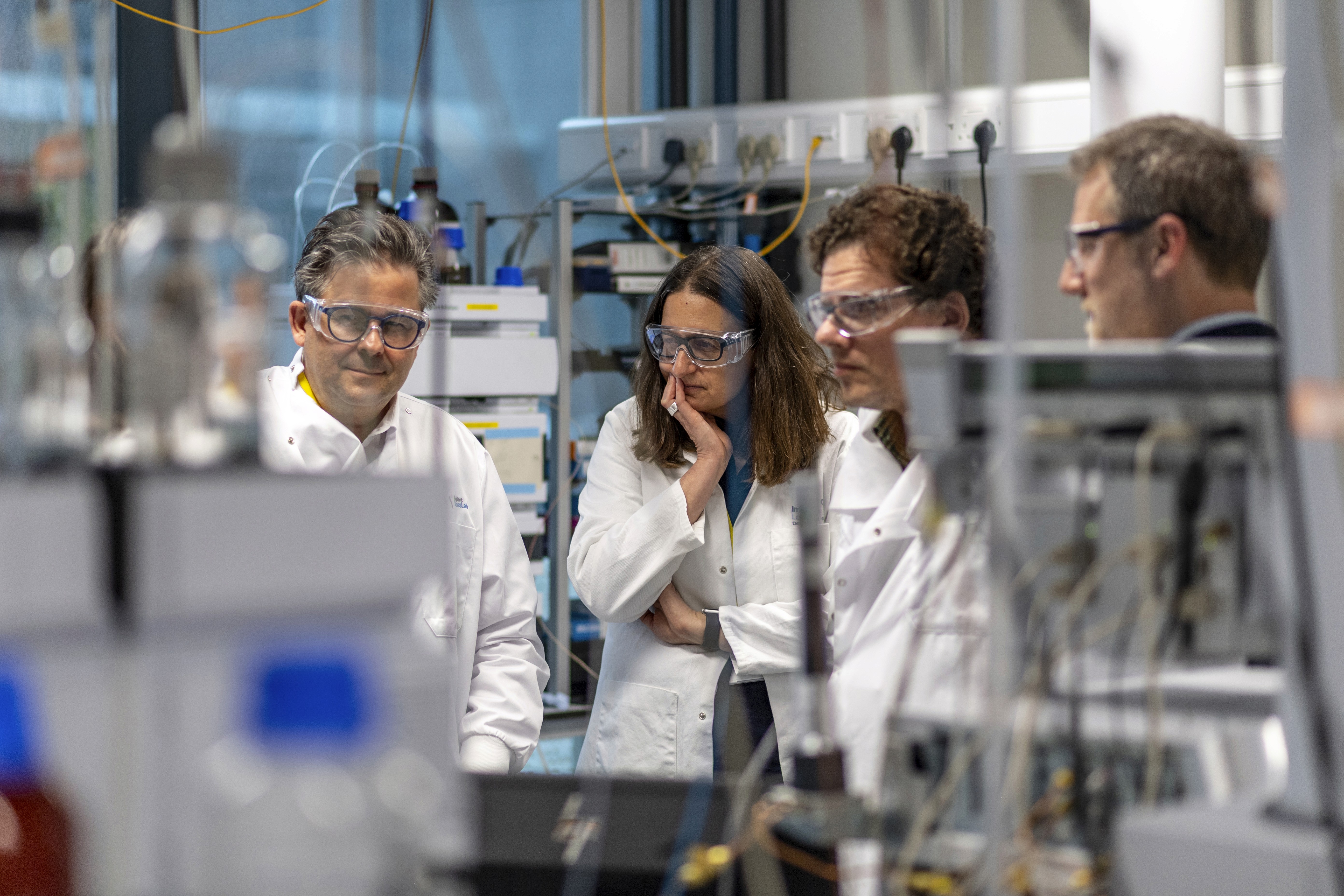
Science Photo Library (Canva)
In the realm of immunotherapy, a promising technique known as CAR T-cell therapy has been making waves. This method, which involves engineering a patient's T cells to better identify and assault antigens on the surface of cancer cells, has been approved for use in the fight against lymphoma and leukemia. However, it's not without its Achilles' heel. Amid the tumultuous battle against cancer, many of these engineered T cells become contaminated with remnants of cancer antigens, leading them to turn their weapons on their own kind. This unfortunate side effect depletes the body's arsenal of cancer-fighting cells, leaving the door ajar for a potential resurgence of the disease.
Yet, a recent study from Yale has shed light on a potential solution to this self-destructive behavior of the engineered T cells. The researchers propose a simple yet ingenious solution: attaching a molecular tail to the engineered T cells used in therapy. This modification, they argue, can curb the cells' tendency to engage in friendly fire. The findings were published recently in Nature Immunology.

Sidi Chen, associate professor of genetics at Yale School of Medicine and senior author of the study, likened the process to "putting a sword back in the sheath after it has done its work."
The Yale team, spearheaded by co-first authors Xiaoyu Zhou and Hanbing Cao, fused CTLA-4 cytoplasmic tails (CCTs) onto the engineered CAR T cells. These CCTs are part of a naturally occurring human protein, CTLA-4, known for its role in keeping the immune system in balance by regulating T cells. The researchers found that the cells equipped with these tails were less fatigued and survived longer than their tail-less counterparts.
Zhou, a postdoctoral associate in Chen's lab, noted that "the CAR T cells with the engineered tails were less reactive but more persistent" in their mission to eliminate cancer cells.
“Utilizing the endocytic feature of the cytotoxic T-lymphocyte-associated antigen-4 (CTLA-4) cytoplasmic tail, we reprogramd CAR function and substantially enhance CAR-T efficacy in vivo.” the authors wrote. “CAR-T cells with monomeric, duplex, or triplex CTLA-4 cytoplasmic tails (CCTs) fused to the C terminus of CAR exhibit a progressive increase in cytotoxicity under repeated stimulation, accompanied by reduced activation and production of proinflammatory cytokines.”
The researchers went on to write that “further characterization reveals that CARs with increasing CCT fusion show a progressively lower surface expression, regulated by their constant endocytosis, recycling, and degradation under steady state. The molecular dynamics of reengineered CAR with CCT fusion results in reduced CAR-mediated trogocytosis, loss of tumor antigen, and improved CAR-T survival. CARs with either monomeric (CAR-1CCT) or duplex CCTs (CAR-2CCT) have superior antitumor efficacy in a relapsed leukemia model. Single-cell RNA sequencing and flow cytometry analysis revealed that CAR-2CCT cells retain a stronger central memory phenotype and exhibit increased persistence.”
Chen believes that it would be a relatively straightforward task for existing companies to fuse CCTs to CAR T cells. He also suggests that these enhancements in therapy could potentially broaden the scope of treatments to include solid tumors.
Chen's affiliations include the Yale Cancer Center, the Yale Stem Cell Center, the Yale Center for Biomedical Data Science, and the Systems Biology Institute and Center for Cancer Systems Biology at Yale’s West Campus. The study was made possible through the support of the National Institutes of Health, the U.S. Department of Defense, and several foundations.