Engineered Human Therapies
Revolutionizing Vaccines and Cancer Treatments with Self-Amplifying RNA
What started as a series of failed experiments has now led to a potential breakthrough in RNA technology, offering hope for future vaccines and cancer treatments
Sep 16, 2024
[Grok]
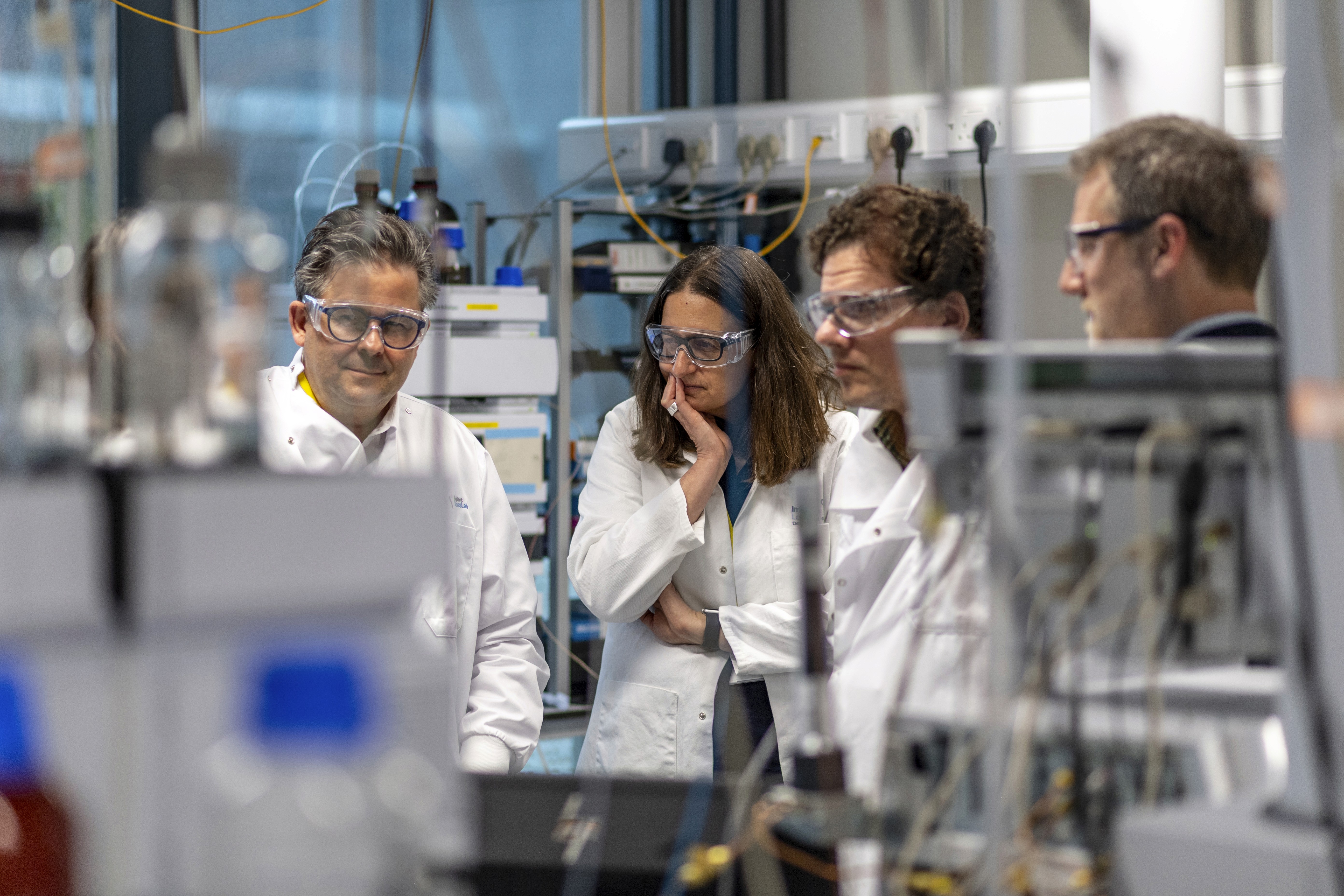
In a Boston University lab, doctoral students Joshua McGee and Jack Kirsch were knee-deep in RNA research, determined to see if small modifications to RNA nucleotides could still function in cellular processes. After dozens of experiments, they hit a wall.
“At first, it was a failure,” McGee admits.
RNA, an essential molecule in living cells, has been the subject of decades of research. It plays a pivotal role in critical cellular tasks—like building proteins, carrying amino acids, and initiating immune responses. More recently, RNA has been harnessed for medical breakthroughs, including treatments for genetic diseases and mRNA-based COVID-19 vaccines. But McGee and Kirsch's work had a bigger goal: using RNA to deliver life-saving drugs and develop more effective vaccines.
Working with Mark Grinstaff, BU’s Distinguished Professor of biomedical engineering and chemistry, and Wilson Wong, an associate professor of biomedical engineering, the team shifted their focus. Rather than abandon the chemical components left from their earlier experiments, they began working with a lesser-known form of RNA—self-amplifying RNA (saRNA). Unlike regular RNA, saRNA replicates itself multiple times within a cell, producing more of the target proteins.
Their persistence paid off. The modified saRNA was successfully replicating itself in a petri dish. McGee recalls their reaction: “A lot of excitement, but also the normal scientist thinking, ‘Did we do this right?’ We went back to do it again and again. And we got the same results.”
This breakthrough launched a yearlong project, taking the research from Grinstaff’s chemistry lab to Wong’s genetics lab and eventually to BU’s National Emerging Infectious Diseases Laboratories (NEIDL). There, they tested their saRNA modification as a vaccine against COVID-19. Remarkably, a lower dose of their vaccine in mice provided the same protection as current mRNA vaccines. Their findings, published in Nature Biotechnology, could be a game-changer in the vaccine landscape.
A New Era for RNA Vaccines
While an saRNA vaccine has already been approved in Japan, the BU team’s modified version has the potential to make the technology more viable for drug manufacturers and overcome challenges associated with saRNA use.
“The challenge with regular self-amplifying RNA is that two competing processes are at play—the RNA is trying to make more protein, while the immune system is degrading it,” explains Grinstaff. Standard mRNA COVID-19 vaccines instruct cells to produce the spike protein, triggering an immune response. An saRNA vaccine goes further, continuously replicating these instructions, which produces more proteins. This means a lower dose could lead to prolonged immune system memory.
“So the idea is that this could give you a long duration of protein expression, even when using a lower dose,” Grinstaff says.
However, saRNA vaccines also pose risks. Their robust protein production can cause stronger side effects, potentially more severe than those seen with current mRNA COVID vaccines.
To address these concerns, the team collaborated with Florian Douam, a virology, immunology, and microbiology assistant professor at BU. His team conducted a “viral challenge,” testing whether the modified saRNA vaccine could offer better protection against severe COVID-19 in mice than earlier vaccines. The results were promising. Their new saRNA vaccine, enhanced with m5C (5-methylcytidine), protected mice from lethal COVID-19 at much lower doses, while triggering only mild inflammatory responses similar to mRNA vaccines.
“There is still plenty of work to be done to unveil all of the advantages of this technology over other existing RNA vaccine approaches,” Douam notes. But the study marks a significant step forward.
Expanding Beyond Vaccines
The potential applications of saRNA extend far beyond COVID vaccines. The BU team believes their modified saRNA could pave the way for innovative treatments and gene therapies.
“At the end of the day, this is a protein-producing system,” says Wong. “A gene-delivery system.”
In gene therapy, saRNA could be programmed to produce missing or defective genes in patients with genetic disorders. For diseases like lung or breast cancer, it could generate anticancer drugs that require high protein production.
“That’s why we’re really excited about our self-amplifying RNA technology,” Wong says. “We think we can lower the dose that’s needed to enable some of these therapeutic applications.”
The groundbreaking potential of saRNA recently earned Grinstaff the National Science Foundation’s Trailblazer Engineering Impact Award, accompanied by a $3 million grant to continue the research. According to the NSF, saRNA could “fundamentally alter the genetic engineering paradigm.”
Reflecting on the journey, McGee emphasizes the importance of perseverance: “There are a lot of publications out there that suggested research on saRNA would also fail. This made me realize that it’s okay to try things that other people think might fail, because, who knows, they could be wrong.”
With the potential to revolutionize vaccine development and beyond, saRNA may be on the cusp of transforming modern medicine.