Meet Anthrobots, Your Body's New Biological Repair Crew
Created from just a single human donor cell, these small-scale biobots offer remarkable healing effects and a glimpse into regenerative medicine's future
Nov 30, 2023
AI Image Created Using DALL-E
In a collaboration between Tufts University and Harvard University's Wyss Institute, researchers have unveiled tiny biological robots crafted from human tracheal cells. Dubbed "Anthrobots," these multicellular robots have demonstrated the ability to move across surfaces and, notably, promote the growth of damaged neurons within a laboratory setting. These patient-derived biobots, showcased in Advanced Science, present potential therapeutic tools for regeneration, healing, and disease treatment.
The Anthrobots build upon earlier research involving Xenobots, multicellular robots created from frog embryo cells. From the laboratories of Micheal Levinwhich, Vannevar Bush, Professor of Biology at Tufts University School of Arts & Sciences, and Josh Bongard at the University of Vermont, the xenobots exhibited navigation capabilities, material collection, information recording, self-healing, and limited replication. The current study takes a significant step forward by demonstrating that these Anthrobots can be constructed from adult human cells without genetic modification, surpassing the capabilities of their amphibian counterparts.
Gizem Gumuskaya, a PhD student involved in the study, highlighted the ability to reprogram cell interactions, enabling the creation of new multicellular structures. “We wanted to probe what cells can do besides create default features in the body,” said Gumuskaya. “By reprogramming interactions between cells, new multicellular structures can be created, analogous to the way stone and brick can be arranged into different structural elements like walls, archways or columns.”
The researchers found that not only could the cells create new multicellular shapes, but they could move in different ways over a surface of human neurons grown in a lab dish and encourage new growth to fill in gaps caused by scratching the layer of cells. While the mechanism behind the Anthrobots' neural growth encouragement remains unclear, the researchers are keen to explore the potential therapeutic applications. “The cellular assemblies we construct in the lab can have capabilities that go beyond what they do in the body,” said Levin. “It is fascinating and completely unexpected that normal patient tracheal cells, without modifying their DNA, can move on their own and encourage neuron growth across a region of damage,” said Levin. “We’re now looking at how the healing mechanism works and asking what else these constructs can do.”
By constructing therapeutic biobots from patients' own, unedited cells, the risk of triggering an immune response and, thus, the need for immunosuppressants is eliminated, and once their work is done, the bots break down and can be reabsorbed by the body. Anthrobot survival outside the body is limited to very specific laboratory conditions, and they are incapable of reproduction, preventing unintended spread. Even under laboratory conditions, they usually survive about 45-60 days before they naturally biodegrade.
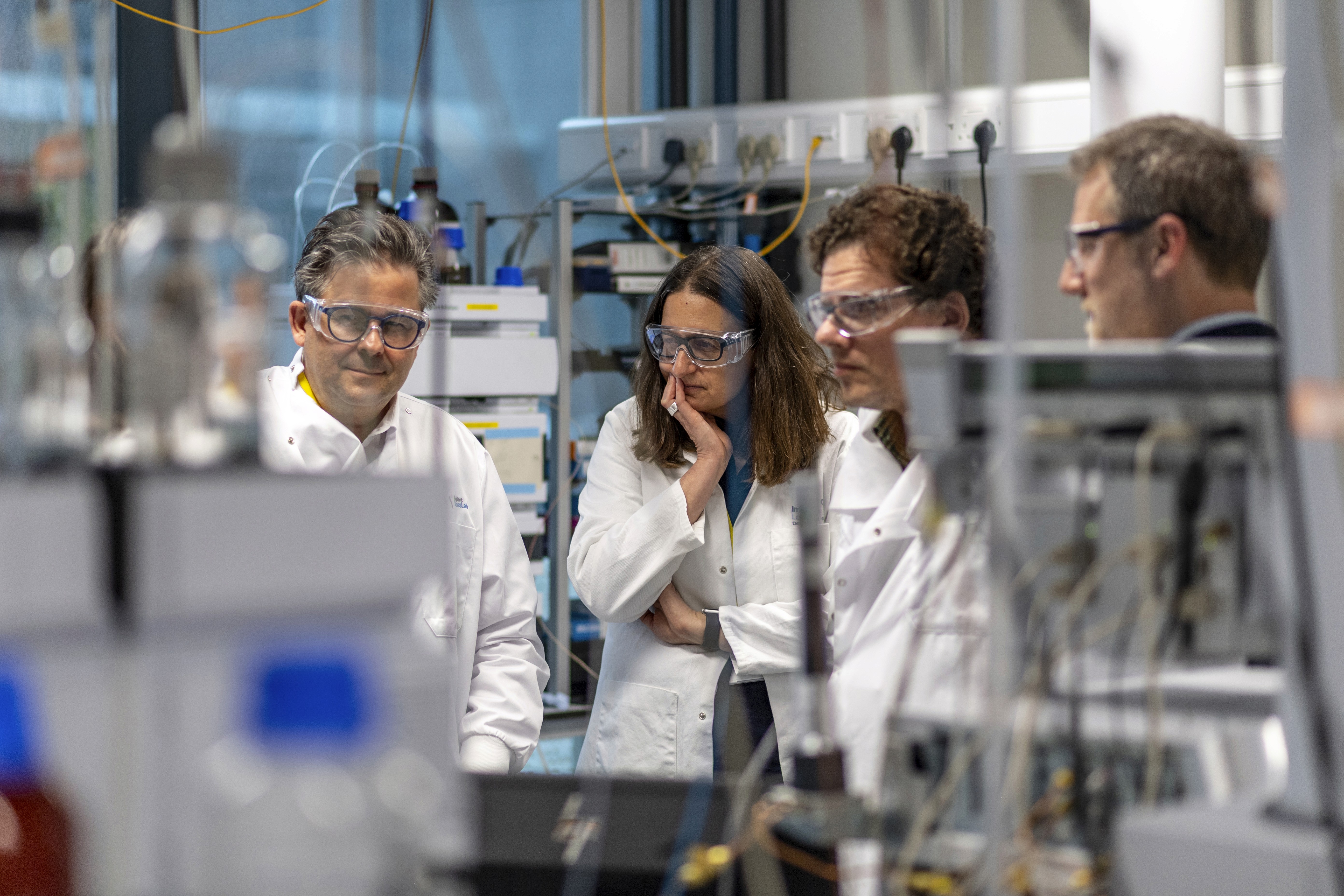
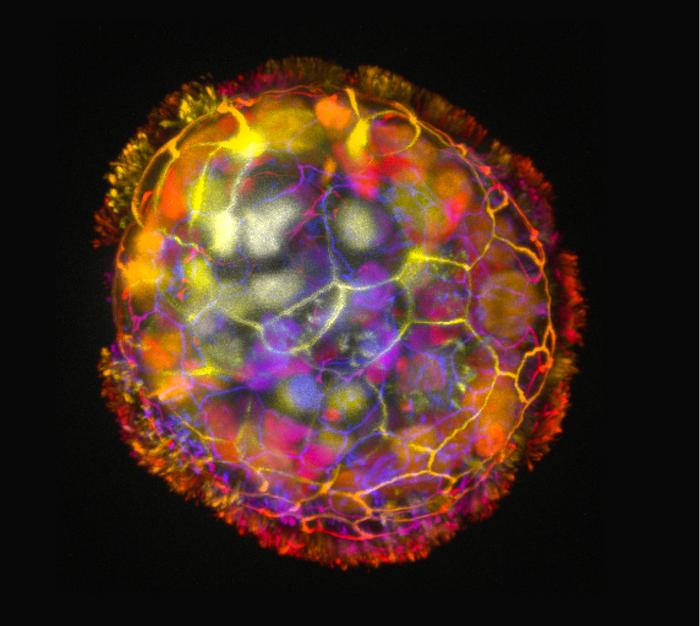
So how are they made? Anthrobots start with a single donor tracheal cell, which comes equipped with hairlike projections called cilia, which will later act as the ‘legs’ of the anthrobots. The tracheal cells spontaneously form multicellular spheres known as organoids when grown in the lab. By imposing specific growth conditions, the researchers were able to prompt the cilia to face outward, eventually resulting in movements reminiscent of oars. “Anthrobots self-assemble in the lab dish,” said Gumuskaya, who created the Anthrobots. “Unlike Xenobots, they don’t require tweezers or scalpels to give them shape, and we can use adult cells – even cells from elderly patients - instead of embryonic cells. It’s fully scalable—we can produce swarms of these bots in parallel, which is a good start for developing a therapeutic tool.”
The Arthrobots produced were extremely varied, ranging in size from the width of a human hair to the tip of a sharpened pencil. Some were spherical and fully covered in cilia, some were irregular or football-shaped with more patchy coverage of cilia, and some were covered with cilia on just one side. They varied in physical characteristics and movement—straight lines, tight circles, wiggles, or any combination of these were observed, depending on cilia distribution. This variation opens avenues for a range of potential future enhancements, allowing Anthrobots to respond to their environment and perform specific functions in the body.
As the researchers plan to apply Anthrobots in therapeutic settings, they conducted lab tests demonstrating the biobots' ability to heal wounds in a layer of human neurons. They grew a two-dimensional layer of human neurons, which they then damaged by scratching with a thin metal rod. Remarkably, a cluster of unmodified Anthrobots (dubbed “superbots” by the researchers) triggered substantial neural regrowth, showcasing their potential to heal live neural tissue efficiently.
This research reveals just how versatile human cells can be without any modification. Looking ahead, the researchers anticipate further developments that could lead to endless applications. In the future, we may see Anthrobots that can ‘hunt’ cancer cells, clear plaque buildup in arteries, repair spinal cord or retinal nerve damage, and deliver targeted drug treatments to aid restoration in damaged organs. As a form of the organoid, these tiny healers could also be used as surrogate patients for personalized drug testing to not only improve patient safety and outcomes but also reduce the need for animal testing.
“The cells can form layers, fold, make spheres, sort and separate themselves by type, fuse together, or even move,” Gumuskaya explained. “Cells can communicate with each other and create these structures dynamically.” As demonstrated by Anthrobots, this flexibility and innate self-assembly not only facilitates the creation of innovative biobots but also deepens our understanding of natural body plan assembly. Understanding the rules that govern how cells assemble and work together in the body can inform the development of regenerative treatments for tissues, organs, and limbs. Gumuskaya went on “We are just figuring out how to combine these elements to create new biological body plans and functions—different than those found in nature.”