Engineered Human Therapies
How Geneticists are 'Base-ically' Revolutionizing Sickle-Cell Treatment
Scientists at St. Jude's, the Broad, and Harvard found base editing increased fetal hemoglobin production in a new treatment for sickle cell disease and beta-thalassemia
Credit: PhonlamaiPhoto Images (Canva)
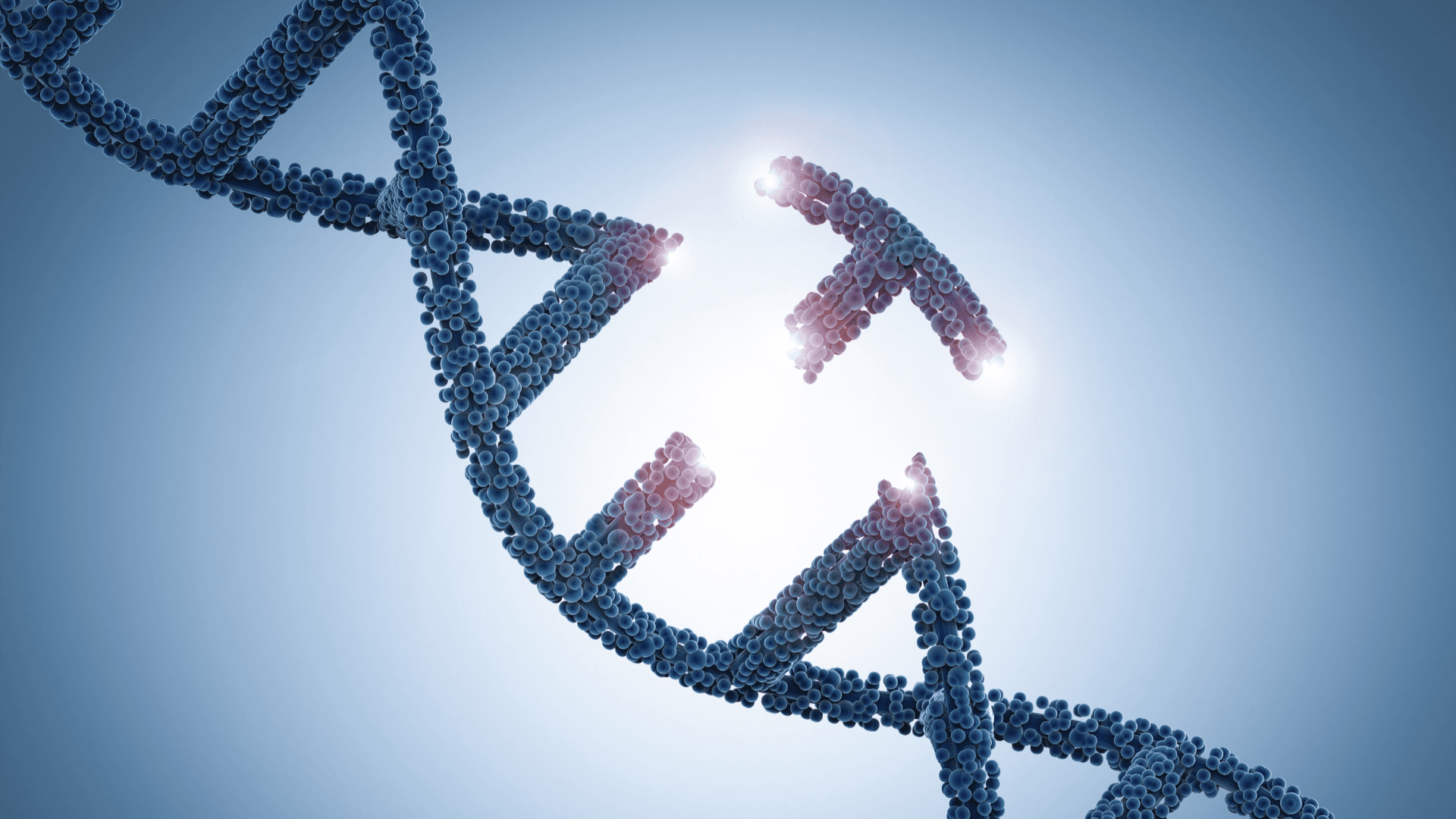
In a significant leap towards treating sickle cell disease (SCD) and beta-thalassemia, researchers from St. Jude Children’s Research Hospital and the Broad Institute of MIT and Harvard are harnessing a cutting-edge gene therapy approach, leveraging next-generation genome editing technology. The work, published in Nature Genetics, focuses on using adenosine base editing to reactivate fetal hemoglobin expression, potentially offering a therapeutic alternative for these prevalent and life-threatening anemias that burden millions worldwide.
SCD and beta-thalassemia result from genetic mutations in adult hemoglobin, the oxygen-transporting molecule in the blood. By reactivating the expression of an alternate hemoglobin subunit typically active in fetuses, scientists anticipate a path to combating these debilitating diseases. The research team utilized the adenosine base editing technology for introducing alterations to the fetal hemoglobin gene, achieving superior and more consistent results compared to other genome editing technologies, such as CRISPR/Cas9 nuclease.
“Base editors meaningfully increase fetal hemoglobin levels,” declared Jonathan Yen, PhD, the lead corresponding author and director of the St. Jude Therapeutic Genome Engineering group. “My team is already hard at work, starting to optimize base editing to move this technology to the clinic.”
The science hinges on the biology of hemoglobin. The adult version, produced after birth, comprises four protein subunits. When mutations occur in the beta-globin gene, disorders like SCD and beta-thalassemia arise. Yet, the human genome also carries the gamma-globin gene, which creates fetal hemoglobin during developmental stages. By leveraging gene editing to reactivate the gamma-globin gene, researchers aim to increase fetal hemoglobin production, compensating for defective adult hemoglobin.
Yen further elucidated, “We used a base editor to create a new TAL1 transcription factor binding site that causes particularly strong induction of fetal hemoglobin. Creating a new transcription factor binding site requires a precise base pair change — something that can’t be done using CRISPR-Cas9 without generating unwanted byproducts and other potential consequences from double-stranded breaks.”
Co-corresponding author Mitchell Weiss, MD, PhD, St. Jude Department of Hematology chair, added, “The gamma-globin [fetal hemoglobin] gene is a good target for base editing because there are very precise mutations that can reactivate its expression to induce expression after birth, which may provide a powerful ‘one-size-fits-all’ treatment for all mutations that cause SCD and beta-thalassemia.”
Boosting fetal hemoglobin production could be a more comprehensive treatment for major hemoglobin disorders, offering potential benefits to most patients with SCD or beta thalassemia, irrespective of their causative mutations. This recent study, in its systematic comparison of different genome editing strategies, has delivered an unprecedented look at the efficacy of these approaches.
David Liu, PhD, Professor at the Broad Institute of MIT and Harvard, and co-corresponding author who pioneered base editing in 2016, said, “We looked closely at the individual DNA sequence outcomes of nucleases and base editors used to make therapeutic edits of fetal hemoglobin genes. Since nucleases often generate complex, uncontrolled mixtures of many different DNA sequence outcomes, we characterized how each nuclease-edited sequence affects fetal hemoglobin expression. Then we did the same for base editing outcomes, which were much more homogeneous.”
Addressing safety concerns, Yen noted, “Base editors may be able to create more potent and precise edits than other technologies. But we must do more safety testing and optimization.” Their study has shown that base editing results in fewer genotoxic events, such as p53 activation and large deletions, demonstrating more consistent and precise edits.
The researchers acknowledge the need for further investigation into the safety of base editing, as some early base editors have been found to cause unintended changes in genomic DNA or RNA at off-target sites.
Emphasizing the importance of testing different genome editing approaches, Weiss said, “It is very important to test and compare different genome editing approaches for treating SCD and beta-thalassemia because the best ones are not known.”
Concurring with Weiss, study co-author and the Cellular and Molecular Therapeutics Branch chief at the National Heart, Lung, and Blood Institute, John Tisdale, MD, highlighted, “The science of gene editing is moving quickly, and we are now able to envision multiple different strategies for combating sickle cell disease. These findings bring us a step closer to our goal of broadly available cures.”
This groundbreaking research propels us forward in the rapidly evolving field of gene editing, taking us closer to the end goal of providing universally accessible cures to treat these prevalent, life-threatening anemias.
Read More
Newletter & More

SynBioBeta
Join the innovators shaping the future with SynBio + AI. From health to ag, materials & more—be part of the revolution.