Engineered Human Therapies
Cancer Therapy Game Changer Could Lie in Bacteria-Based Chemo
A new study from NUS Medicine reveals a revolutionary approach to chemotherapy, significantly reducing side effects and improving drug efficacy
Jun 10, 2024
[DALL-E]
In the ongoing battle against cancer, traditional chemotherapy has long been a double-edged sword, offering a vital lifeline but at the cost of severe side effects, collateral damage to healthy tissues, and often limited efficacy.
Enter a groundbreaking advancement from the researchers at the Yong Loo Lin School of Medicine, National University of Singapore (NUS Medicine). They have unveiled a transformative approach to cancer therapy—one that promises to be more targeted, effective, and far less toxic than conventional methods. This novel technique not only enhances the potency of treatments but also significantly reduces the required dosage of chemotherapy drugs.
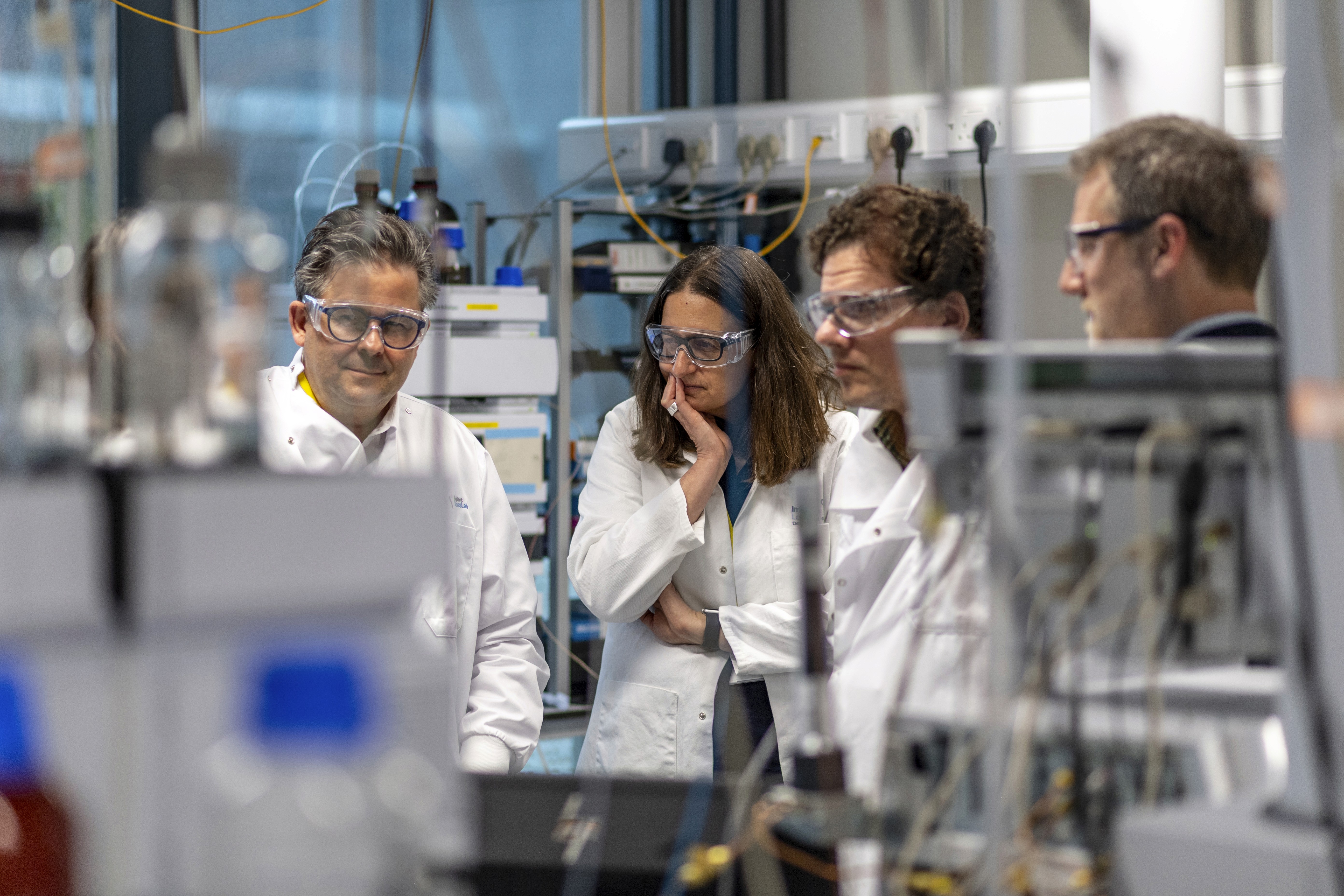
Under the leadership of Associate Professor Matthew Chang, the team at the NUS Synthetic Biology for Clinical and Technological Innovation (SynCTI) and the Synthetic Biology Translational Programme (Syn Bio TRP) has pioneered a new drug delivery system that could revolutionize cancer treatment. Published recently in Nature Communications, their findings introduce an innovative method that delivers chemotherapy drugs directly to tumor sites by leveraging the natural interactions between bacteria and cancer cells.
This new method centers around prodrugs—inactive molecules that become active within the body, particularly in the unique conditions of tumor environments, such as low oxygen or high acidity. This activation at the cancer site minimizes harm to healthy tissues. While current prodrug strategies often lack precise targeting and rely on complex carriers, the researchers at NUS Medicine have overcome these hurdles with a novel approach.
The team developed a prodrug delivery system using a commensal Lactobacillus strain that specifically binds to cancer cells through a surface molecule called heparan sulfate. These engineered bacteria carry a prodrug that converts into the chemotherapy drug SN-38 directly at the tumor site. In preclinical models of nasopharyngeal cancer, the engineered bacteria localized precisely in the tumor, releasing the drug and reducing tumor growth by 67% while increasing the drug's effectiveness by 54%.
What makes this research particularly promising is its potential applicability across various cancer types. The Lactobacillus strain identified by the researchers binds specifically to cancer cells, opening doors for a broader range of treatments. Dr. Shen Haosheng, Research Fellow at SynCTI, emphasized this potential: “By harnessing the affinity between bacteria and cancer cells, we aim to revolutionize chemotherapy delivery. We are evaluating the binding affinity of several microbial strains to multiple cancer cell lines with the aim of developing a versatile delivery system using microbial strains to target chemotherapy drugs for various mucosal cancers, such as colorectal, bladder, stomach, oral, lung, and nasal cancer.”
Associate Professor Chang, Dean’s Chair in Medicine and Director of SynCTI and NUS Medicine Syn Bio TRP, added: “Cancer treatment often takes a tremendously heavy toll on patients. Our research represents a significant step toward developing a more targeted and less toxic approach to fighting cancer. We hope this can pave the way for therapies that are both mild and effective.”
In the fight against cancer, these pioneering efforts from NUS Medicine may well signal a new era of hope and healing, transforming the landscape of cancer treatment with precision and compassion.